8.12.1. Community Pharmacy
A Community Pharmacist is the most readily available healthcare
professional, with contact being made outwith an appointment being made.
They can also be seen at weekends.
CDs will be ordered from a local wholesaler and stored securely in the
pharmacy before supplying to patients. Access to CDs should be stored
appropriately and access to the CD Cabinet should be restricted.
Similarly, access to the keys to the CD Cabinet should also be restricted.
CDs should not be stored out with the Cabinet unless under the direct
personal control of the Pharmacist.
Methadone (Schedule 2) and Buprenorphine (Schedule 3) are CDs often
prescribed in instalments to substance misuse patients and complications
can arise where the pharmacy is closed, for example at weekends or at bank
holidays, if the prescription is not appropriately written.
The Home Office has provided some recognised wording which can be appended
to the prescription to help avoid these difficulties. All instalment
prescriptions for CDs including, for example, those supplied in monitored
dosage systems are subject to the same legal requirements.
Pharmacists may also supply other professionals with CDs including GPs who
may order them from a community pharmacy for use in their practice. Orders
for CDs within the NHS will be written on controlled stationery (GP10A).
A CD Register is required to record all transactions involving Schedule 2
drugs. Some Community Pharmacies now use an electronic CD Register. During
a CD destruction, the Authorised Witness must log into the system
following the Pharmacist to confirm CDs have been destroyed. The
Authorised Witness must log out of the electronic Register before leaving
the Community Pharmacy.
Community Pharmacies are inspected by the General Pharmaceutical Council
Inspectorate, not by the CD Team, however, the team will provide support
and guidance regarding all CD matters. It is also a legal obligation to
share information and have regular communication between each professional
body regarding any incident/issues/concern.
8.12.2. Controlled Drug Prescriptions in Community
It is the responsibility of the patient to collect their Controlled Drugs
from the Community Pharmacy. In situations where this is not possible,
arrangements should be made by the patient to have the Community Pharmacy
deliver their medication. Only in exceptional circumstances, e.g. urgent
requirement to administer medication, should the practitioner organise to
deliver the Controlled Drugs themselves.
The person collecting the medicine from the dispensing Pharmacy will be
required to sign the back of the prescription form when collecting
Schedule 2 or 3 CDs. Legislation states that the Pharmacist must ascertain
whether the person collecting is the patient, patientís representative or
healthcare professional. If the person collecting the Schedule 2
Controlled Drug is a healthcare professional acting in their professional
capacity on behalf of the patient, the Pharmacist must also obtain the
name and address of the healthcare professional and evidence of identity
(unless he/she is acquainted with that person).
If a patient wants a representative to collect a dispensed CD on their
behalf, Pharmacists are advised to obtain a letter from the patient that
authorises and names the representative. This also includes those detained
in Police custody who should supply a letter of authorisation to a police
custody officer to present to the Pharmacist).
A separate letter should be obtained each time the patient sends a
representative to collect and the representative should bring
identification with them. The Pharmacist must be certain that the letter
is genuine.
It is good practice to insist on seeing the patient at least once a week
unless this is known not to be possible.
The record of supply in the CD Register must include the details of the
patientís representative.
If the prescription states the dose must be supervised, the Pharmacist
should contact the prescriber before the medicine is supplied to the
representative as the supervision will not be possible. It is legally
acceptable to confirm verbally with the prescriber that they are happy
with this arrangement as supervision is not a legal requirement under the
Misuse of Drugs Regulations 2001
http://www.legislation.gov.uk/uksi/2001/3998/contents/made.
It would not be necessary for the Pharmacist to contact the prescriber if
the patient has been detained in Police custody and the representative
collected would be a police custody officer or custody healthcare
professional. This is because the administration of any CD in custody will
be supervised by a healthcare professional.
If the dose is usually supervised, but has been supplied the Pharmacist
should consider annotating the prescription and patient mediation records
to advise other that the dose has not been supervised in Pharmacy.
It is good practice for the person collecting the CD to sign the space on
the reverse of the prescription form, specific for this purpose. A supply
can be made if this is not signed, subject to professional judgement by
the Pharmacist.
Instalment prescriptions need only be signed once.
A representative, including a delivery driver, can sign on behalf of the
patient, however, a robust audit trail should be available to confirm
successful delivery of medication to the patient.
8.12.3. Administration of Controlled Drugs in the Community
Controlled Drugs may only be administered to patients in accordance with
the directions of the qualified practitioner in charge of the patient.
A Registered Nurse or Doctor in the community may administer, without
witness, a CD which has been obtained on prescription by the patient. A GP
may administer a CD from stock.
In this case, an entry must be made in the appropriate CD Register.
A prescriber may complete a Controlled Drug record form, authorising the
community nurse to administer a particular CD. A record of that
administration must also be made on the accompanying form.
The following process must be followed:
∑
Check the identity of the patient. The patient's name and date of birth
corresponds with the prescription and wherever possible is confirmed by
the patient.
∑
Check the patient is not allergic to the medicine prior to administration.
∑
Ensure that the intended drug and dose for the patient is correct.
∑
Know the therapeutic uses of the medicine to be administered, its normal
dosage, side effects, precautions and contra-indications.
∑
Check the prescription and/or the label on the medicine dispensed is
clearly written and unambiguous.
∑
Check the expiry date of the medicine.
∑
Check the strength, dosage, weight, where appropriate method of
administration, route and timing, frequency, start and finish dates.
∑
Contact the prescriber or another authorised prescriber without delay
where contra-indications to the prescribed medicine are discovered, where
the patient develops a reaction to the medicine, or where assessment of
the patient indicates that the medicine is no longer suitable.
∑
Where a nurse is administering a Controlled Drug that has already been
prescribed and dispensed for that patient, obtaining a witness and second
signature must be based on the local risk assessment.
∑
Although normally the second signatory should be another registered health
care professional, in the interest of patient care, where this is not
possible a second suitable person who has been assessed as competent may
sign e.g. Student Nurse or family member.
∑
A stock check of Controlled Drugs must be taken and recorded as part of
the administration procedure.
8.12.4. Recording Administration of CDs in the Community
CD administration must be entered in the relevant CD Register. In the case
of administration within a patientís home, the practitioner performing the
administration must complete the record sheets and stored in the patient
held record. The full
signature must be recorded of the person who administered the CD and the
person who carried out the check with the patientís name and the time the
dose was administered. Where CD was not given, refused or dropped, this
information must be clearly recorded in the CD Register. Entries and
errors must be indelible and must never be altered or obliterated.
Any errors must be bracketed and the correct entry made in an adjacent
space or next line. A brief explanation eg entered in error must be made
in the margin or at the bottom of the page and then signed and dated.
Pages or part pages must never be torn out of the Register.
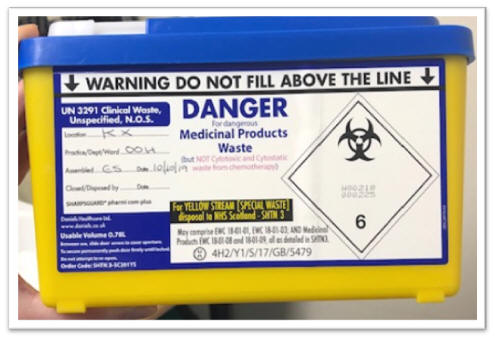
When only part of an ampoule containing CD is used, or dose
refused/dropped, this is placed into a 0.78l Pharmacy blue lidded
pharmaceutical waste container (held within OOH GP CD bag). Vernagel
sachet is added to each bin to absorb the discarded liquid. The amount
discarded must be recorded appropriately in the correct CD Register. Where
there is a witness to the administration, this person must also sign the
CD Register as witness to the destruction/ discard.
Any errors or incidents in relation to the administration of CDs must be
recorded and reported via the relevant manager and a DATIX entry
submitted. This must also be detailed in the patientís record.
8.12.5. NHS Tayside Drug and Alcohol Recovery Services
The NHS Tayside Drug and Alcohol Recovery Service is responsible for
providing specialist clinical services to patients and professional
support to Community pharmacies and prescribers in all aspects of
substance use.
The CD Team work closely with the local Drug and Alcohol Recovery teams to
ensure legal requirements are met and that the highest standards of the
service provision are delivered.
8.12.6. Patients on Opioid Replacement Therapy who are Admitted or
Discharged from Hospital
Patients who are receiving prescribed Methadone or Buprenorphine for
opiate dependence in the community may be dispensed instalments daily or
on a weekly basis by their Pharmacist. Consumption of the dose may be
supervised by the Pharmacist. Frequency of dispensing takes into account
the individual patientís dose, stability and personal circumstances.
8.12.7. On Admission
Contact the patientís Community Pharmacist or
NHS Tayside Drug and Alcohol Recovery Service
to confirm that the patient is prescribed Opiate Replacement and to inform
them of the admission. Obtain the following information:
∑
Current dose.
∑
If on supervised or daily pick-ups.
∑
When last dose was dispensed / supervised.
∑
Number of days supply given (if not daily dispensing).
Patientís Own CDs must be stored appropriately (see Section 8.15.1.).
On admission to Hospital, Patientís Own liquid CDs should only be used in
exception circumstances as the contents cannot be checked.
8.12.8. On Discharge (Nurse or prescriber dealing with patientís
discharge)
Contact the GP or NHS Tayside Drug and Alcohol Recovery Service to
inform them of the agreed discharge date and time, confirming the current
dose and when the last dose will be administered before discharge.
Confirm that the Prescriber will make the necessary arrangements with the
Community Pharmacist to provide a new prescription or re-instate the
suspended prescription. If the Prescriber is not available contact the
Community Pharmacist directly for who should be able to advise whether a
community prescription is still current and to agree arrangements for
continuation and when next dose is due.
Administer the daily dose on the Ward before the patient is discharged,
unless alternative arrangements have been made. Inform the patient of the
arrangements for the next dose.
Do not return any unused supplies that were brought in on admission, and
do not provide a discharge supply unless a supply is required until the
regular arrangement in the community is put in place (for example, over
holiday weekends).